An Incubator for Ideas
Margaret’s life isn’t easy. Now 72, the widow has lung, kidney, and heart problems related to diabetes. In recent months, she’s been admitted to the hospital five times. After she’s discharged, she resumes life as best she can, aided by her pregnant daughter, until her health worsens once again.
A small group of Emory nursing students have come to know Margaret. They’ve seen her in the doctor’s office, at the hospital, at home, and in her neighborhood — all without leaving the classroom. They entered her world after donning a virtual reality (VR) headset to test a program developed by Emory nursing professor Beth Ann Swan, PhD, RN, FAAN, and her team.
Swan devised the VR program to teach students about hotspotting. The health practice approach targets “super utilizers”— frequent users of health care services like Margaret — to reduce the disproportionately high cost of their care by addressing their complex medical and social needs.
To develop the program, Swan collected data on Emory Healthcare patients through Project NeLL, an electronic learning library that provides nursing faculty, researchers, students, and nurses at Emory and other U.S. locations with access to vast stores of patient data. Swan sorted through the data to create Margaret and four other diverse virtual patients.
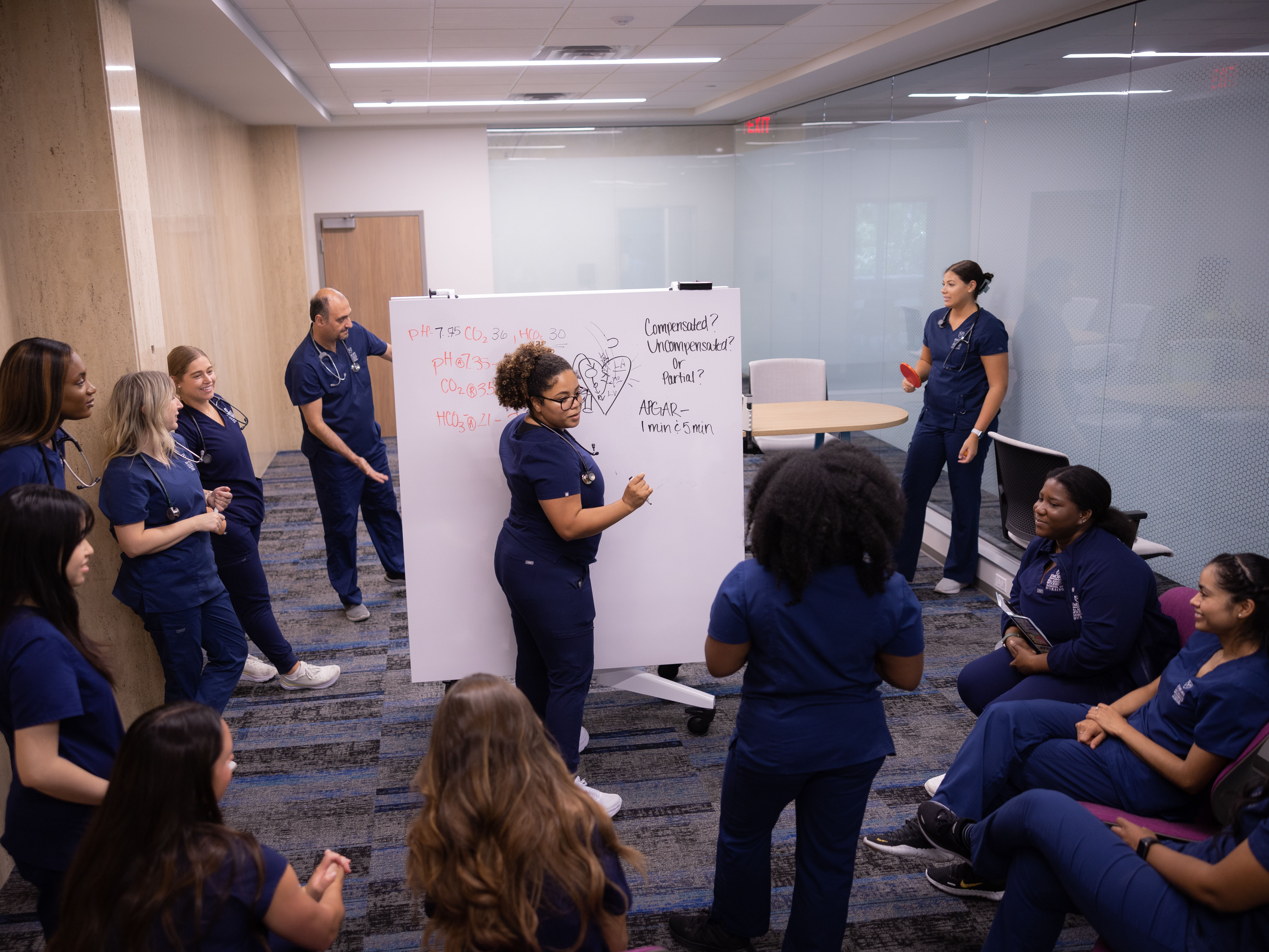
The project is one of many that faculty believe will come to life in the Innovation Hub at the Emory Nursing Learning Center. Located at the top of the staircase on the second floor, the hub is a place “where ideas will collide,” says Swan, executive director of the ENLC. “It will serve as an incubator space where students will learn to think outside the box. How that takes shape might depend on the day and how they end up using that space.”
The rectangular-shaped hub has glass walls, white boards, and movable furniture designed to ebb and flow with the ideas that take shape there. Students of all levels, from BSN to PhD, will use the space to collaborate with School of Nursing faculty and scientists, Emory Healthcare nurses, and technology and industry experts to design and test a host of ideas. Among them: phone apps, patient care devices and sensors, artificial intelligence (AI) and machine learning programs, and nursing workflow systems.
Their ideas will align with the nursing school’s Innovation Strategic Initiative. Led by Swan, the initiative provides a framework for projects in digital health technology, care delivery, simulation, design thinking, and computational health sciences.
EDUCATING INNOVATIVE NURSES

“I decided to go to Emory because I knew I would get a strong clinical foundation in nursing, and that’s what I was looking for,” says Masunaga.
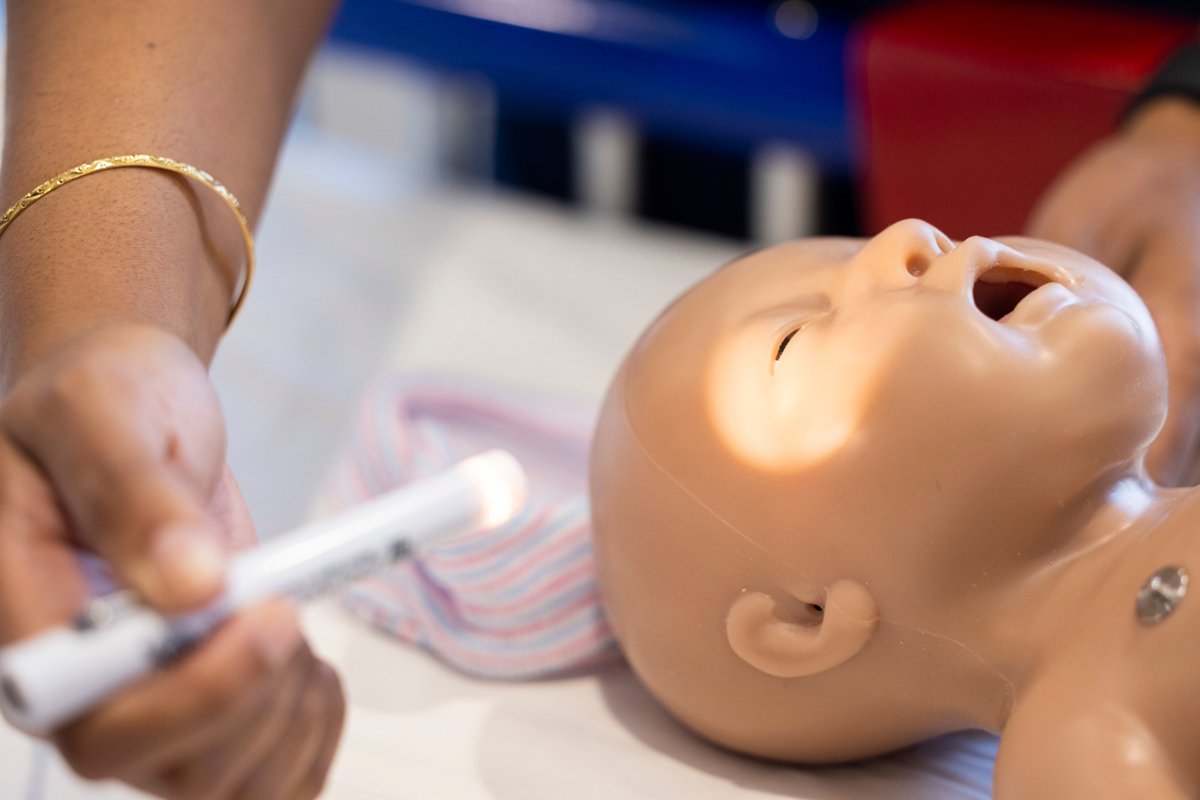
She is well on her way. This past summer, she completed a pediatric and maternity rotation at Emory Decatur Hospital, which proved both eye-opening and fulfilling.
“I felt so connected to expectant and new mothers and their babies,” she says. “Where I come from, we have very low access to health care. When my mom was planning to have me, the plan wasn’t about which hospital to go to. The plan was how to get to another island with acute care services in case something went wrong. Being in a health system like Emory’s, which has so many resources and so much innovation and research going on, is just amazing.”
Masunaga has been exploring her innovative side as part of a research team led by biomedical engineer Xiao Hu, PhD, associate director of the school’s Center for Data Science.
More than 10 years ago, as a faculty member at UCLA Neurosurgery, Hu developed an algorithm to help prevent nurse alarm fatigue. Typically, ICU monitors emit a host of alarm sounds, many of them false or non-life-threatening. His solution was to create a super alarm, a learning software that captures trending patterns, filters out false alarms, and more critically identifies clusters of alarms that co-occur consistently as harbingers of impending patient events. When a super alarm sounds, it indicates when a patient truly needs attention, such as when the heart or lungs begin to malfunction.
Hu has refined the algorithm to perform more effectively: It works by combining data from a bedside monitor and an electronic health record to look for patterns in a patient’s condition and treatment over time.
How does it work? Consider a male hospital patient who is experiencing cardiac arrhythmia. Meanwhile, two hours earlier, his electrolytes showed a minor imbalance.
“The algorithm can put the two factors together,” Hu explains. “The patient’s heart is not beating well because of an electrolyte imbalance. This information gives clinicians a more precise picture of cardiac arrhythmia to explain why it’s abnormal.”
In another instance, a patient’s heartbeat interval is longer than on the previous day. The electronic health record shows the patient is on an anti-arrhythmia drug that elongates the heartbeat interval.
“The challenge is the information is there, but in two or even more different systems,” Hu says. “It takes time and attention to pull the information together. That’s where machine learning comes in. It can put existing data together to determine where the patterns matter.”
Masunaga is interested in learning how biomedical engineers and computer scientists work together to build algorithms like the one Hu has developed. In particular, she will look at how to improve nurses’ charting process so the data they enter will help the algorithm learn better.
“Nurses spend the most time with the patient,” says Masunaga. “They’re the ones who document any changes in a patient’s status.”
Going forward, the Emory Nursing Learning Center will enable Hu to test the algorithm and other projects in a simulated hospital setting. In the Innovation Hub, he can gather clinicians and industry experts together to solicit their feedback on current and future projects.
“The learning center,” he says, “will allow us to mature our algorithm so it can gather information to let nurses know when and how to intervene quickly to help their patients.”