A Pioneer in the ED
By Laura Raines

Dian Dowling Evans taught and mentored Chris Martinborough. He now works as an ENP at Emory University Hospital Midtown.

As a psychologist working for the Georgia Department of Vocational Rehabilitation, Dian Dowling Evans 90MSN PhD FAANP noticed that her clients told nurses more about themselves than they did her.
|
|
• Shared Vision, Shared Success• The Right Fit• Continuing Education for All• A Pioneer in the ED Creating new models of care• Erasing the Data Dread |
|
|
|
“It was an ‘ah-ha’ moment,” recalls Evans, clinical professor and specialty coordinator of the Emergency Nurse Practitioner (ENP) program at Emory. “I realized that if I became a nurse, I’d have more skills to help the whole person. It’s the best career decision I’ve ever made.”
She discovered her niche working as a staff nurse in the emergency department (ED) at Athens Regional Medical Center in northeast Georgia. But when she asked her mentor, Chip Pettigrew MD, if he would consider hiring her as a nurse practitioner (NP) after she completed her MSN degree at Emory, he wasn’t sure how an NP would be accepted in emergency medicine. At the time, NPs in the Athens community mostly worked in public health and rural clinics. Undaunted, Evans requested a clinical rotation with him in the ED and offered to do thesis research that would benefit the department.
“I went through a three-foot stack of patient charts spanning a month to gather data on census volumes, patient acuity levels, and patient-to-provider staffing ratios,” she says. “I found that 68 percent of our ED patients had lower acuity and primary care problems and could be seen by an NP. As an NP, I would be qualified to care for these patients and relieve the physicians to care for more seriously ill and injured patients. Dr. Pettigrew agreed and offered me a job.”
Thus, Evans became the first NP to be granted hospital privileges at Athens Regional Medical Center and the first NP to work in the emergency department. Since launching her advanced practice career in 1991, Evans has seen enormous changes in emergency care and served at the forefront of advancing ENP training and practice.
|
|
In the 1980s, only one university offered an ENP program. At the time, NPs working in emergency care primarily were trained on the job by physicians. By the 1990s, on-the-job training became difficult. “Census levels in emergency departments increased by 28 percent in the ’90s and have increased by 2 to 3 percent annually ever since,” says Evans. “The ED has become the safety net for patients without access to care. It’s also become the way most patients are admitted to the hospital.”
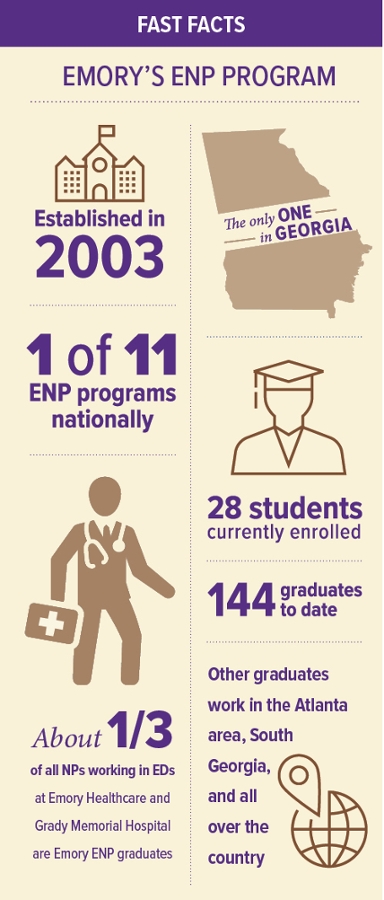
In 2003, Emory started its ENP program as the second accredited integrated family nurse practitioner (FNP) and emergency nurse practitioner program in the country. Graduates of the program must first certify as an FNP before they can sit for specialty certification as an ENP. Evans has served as ENP specialty coordinator since 2009.
“It’s the best job I’ve ever had and the most challenging,” she says. “As an educator, I’m 100 percent committed to my students to ensure they receive quality training and mentorship in what is a high-stakes nursing specialty. That’s what my mentor did for me.”
Typically, ENPs might care for 20 or more patients, of all ages and acuity levels, per shift. While ENPs are grounded in practicing team-based care and working collaboratively with physicians, they must be prepared to work autonomously when ED levels surge during flu season or a mass casualty.
ENP preparation builds on the FNP curriculum with added content in urgent and emergent medical care. Evans’ students also learn basic and advanced procedural skills, including airway management and cardiac resuscitation, central line insertion, advanced wound repair, fracture care and splinting, and delivering babies in the ED. They also learn how to interpret X-rays and other diagnostic tests. Students acquire these skills through labs, simulation exercises, and 750 to 800 hours of clinical rotations.
Emory’s ENP program is the only one in the country that formally trains NPs with emergency medicine physician residents in a specially designed clinical rotation at Grady Memorial Hospital. Research by Kate Heilpern MD FACEP, former chair of Emory’s Department of Emergency Medicine, and Evans has shown that this type of training better prepares students for the team environment of emergency settings. Their interprofessional training model is now an exemplar for preparing a high-quality emergency care workforce.
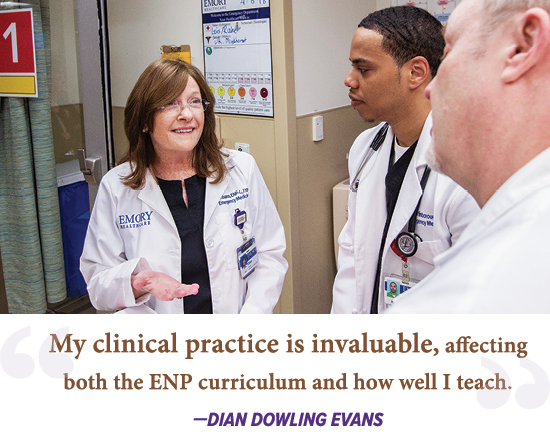
Evans maintains a clinical practice in the ED at Emory University Hospital to complement her teaching. “I don’t think you can lead a clinical program without practicing in health care today,” she says. “Things change too fast. If I’d stopped practicing when I started teaching, I’d be so out of the loop. My clinical practice is invaluable, affecting both the ENP curriculum and how well I teach it.”
Being taught by working faculty was one of the key attractions of Emory’s ENP program for Chris Martinborough 17MSN FNP-C ENP, who began his career in the ED at Emory University Hospital Midtown this past spring. He values the lessons his instructors shared from their own practice.
“Dr. Evans told us to always look at a patient’s skin before doing an initial exam. You can miss certain things if you don’t,” he says. “Even if you are rushed, you look at the patient. Sight comes first.
“She understands that every student’s learning style is different,” he continues. “She uses different ways to present and have us experience the material, so that we really learn. She wants us to succeed. I passed my board exams more easily than I expected thanks to such good preparation.”
Evans advocates for her graduates and others in the workforce nationally. She co-founded the American Academy of Emergency Nurse Practitioners in 2014, serving as executive chair for two years, and has served on committees to set the standards and process for ENP board certification.
Currently, about 14,000 NPs work in emergency departments, and demand for these specially trained nurses is growing.
“We’ve been working on national policies regarding practice and curriculum standardization,” Evans says. “We anticipate that within 10 years a nurse practitioner will have to be ENP board-certified to work in the ED. We’re raising the bar, and that will be good for public health.”
She’s proud of the growth in her specialty and her part in preparing future providers. “I think we’re going to be in good hands,” she says.