A Nurse Going Above and Beyond
By Roger Slavens
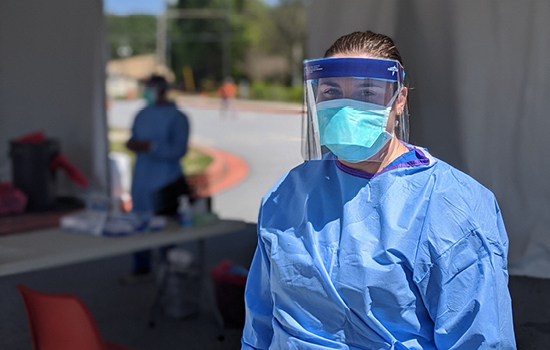
In addition to helping COVID-19 patients in the emergency room, Lindros has played an instrumental role in calling up volunteers from the Fulton County Medical Reserve Corps to help with drive-through testing.
“One of the main reasons why I chose Emory for nursing school was because of how well the nurses and doctors handled the Ebola outbreak starting back in 2014,” she says. “I thought when I came to Emory that at some point I would be trained to be part of the response team to a similar outbreak in another country. But never did I ever think it would be happening in the U.S., right here in Atlanta, right now.” |
|
Kayla Lindros 18N is more eager than most for the world to return to some sense of normalcy during the COVID-19 pandemic. After all, as an emergency department nurse, she’s been caring for infected patients for months and she’s seen some of the worst the coronavirus can do. But as more states open up, Lindros and many of her counterparts worry that we’re moving too fast—and that the general public will take it as a cue to drop their guard too soon.
“Those who don’t know they have COVID-19, people who are asymptomatic, are now going back out and not taking enough precautions,” says Lindros, who works at Grady Memorial Hospital. “They don’t realize they are still putting others at significant risk and getting others sick. They don’t see what we see here in the emergency rooms and the ICUs.”
“People of all ages and backgrounds—many with underlying medical issues but many who were otherwise healthy—are coming into hospitals with severe COVID-19 symptoms and being put on ventilators,” she says. “Some of them will wind up dying, and when they die in a hospital, they frequently do it alone. Visitation is tightly restricted because of the high risk of infection. My colleagues and I have often had to deliver the bad news to families; we’re the ones who tell them they can’t even come in to say goodbye to their loved ones.”
When she’s able, Lindros allows patients to borrow her iPhone so they can FaceTime with their spouses or kids so they don’t feel so alone. “Even if they’re not dying, I still see COVID-19 patients isolated and afraid,” she says. “When they do have human contact, it’s with doctors and nurses and specialists coming in gowns and goggles—they can’t even see our faces. We see this every day and it’s demoralizing, but in a way it’s also motivating because it drives us to help them get better and get out of the hospital and get back home.”
TREATING PATIENTS STARTS IN THE ER
Grady Memorial Hospital, located in downtown Atlanta, has always been a high-volume hospital, with nearly 1,000 inpatient beds, Lindros says. “We treat a lot of the underserved, underinsured population,” she says. “But on top of our typical patient load, we’ve been hit hard by the surge of people throughout Fulton and DeKalb counties who have come in to be treated for COVID-19 symptoms.”
“We screen everybody that comes into the hospital through the emergency department,” she says. “We take a full set of vital signs and then ask them if them about their symptoms. Based on our assessment, we determine if they should be put in our respiratory emergency service area, where doctors and nurses will give them a much more thorough work up and determine if they need to be admitted, or if they can be discharged home with self-isolation instructions.”
During these past few months to cover these waves of patients, Lindros has been asked to work far more than she ever has. “At the worst of it—when our hospital has been full with regular patients and COVID-19 patients—I’ve worked twelve-hour shifts five or six days a week,” she says. “Luckily they’re rotating us through different departments so we don’t burn out. Not only am I doing the work of an emergency department head nurse, but also an ICU nurse, a step-down nurse, often all on the same shift. So I’ve had to shift gears a lot.”
DRIVE-THROUGH TESTING: VOLUNTEERS MAKE IT HAPPEN
Despite being overworked and stressed more than normal, Lindros’s work fighting COVID-19 doesn’t end at the hospital. She also serves as co-chair of the Fulton County Medical Reserve Corps, a group of clinical and nonclinical volunteers that helps respond in emergency situations such as a disease outbreak or a natural disaster. Through the corps, she’s playing a key role in increasing the amount of coronavirus testing being conducted by Fulton County.
“Fulton County, the Georgia Department of Public Health, and Emory Healthcare have set up drive-through testing areas so people who’ve been referred by their physician, can get swabbed by nurses and physicians—most of them volunteers—without flooding emergency rooms and risking further exposure.
While Lindros donates her precious free time to conduct some of the swabbing herself, but her main focus is as a liaison between the Fulton County Medical Reserve Corps and the state and county agencies. She also helps organize the volunteer response, making sure they’re properly trained for whatever crisis Fulton County is facing. Once a COVID-19 vaccine has been developed, she hopes to help coordinate the mass vaccination campaign that will follow in the county.
It was no random coincidence that she got involved, however. Lindros admits that she’s long been fascinated by infectious diseases and how hospitals and health care organizations leap to respond to outbreaks.
“One of the main reasons why I chose Emory for nursing school was because of how well the nurses and doctors handled the Ebola outbreak starting back in 2014,” she says. “I thought when I came to Emory that at some point I would be trained to be part of the response team to a similar outbreak in another country. But never did I ever think it would be happening in the U.S., right here in Atlanta, right now.”
While Lindros still worries about a certain percentage of the population putting us two steps back in the battle against the coronavirus, she says that for the most part, she’s been overwhelmed with the support she’s seen from the general public. “So many people have stepped forward to help us out by following the guidelines or even going beyond to sew masks and donate food to hospitals,” she says. “For the most part, it’s like you’re witnessing something new—a sense of community that wasn’t apparent before—as people have stepped up to really support health care and other essential workers. It makes me feel so good as a human being.”
